Abstract
Introduction: Febrile neutropenia (FN) is a serious complication among patients receiving myelosuppressive chemotherapy (MC). Clinical trials have shown efficacy of primary prophylaxis with granulocyte colony-stimulating factor (PP-GCSF) in reducing FN risk, but few population-based studies have examined trends in PP-GCSF use and FN incidence in older patients over the past 20 years. We describe trends in MC regimens by FN risk category, PP-GCSF use, and risk of neutropenia (NP)-related hospitalization focusing on older NHL patients initiating MC.
Methods: We identified patients (age ≥ 66 years) diagnosed with NHL and initiating MC each year 1995-2015 using Medicare 5% (1994-2007) and 20% (2007-2015) sample data. We required patients to be continuously enrolled in Medicare Part A and B for 12 months before MC initiation (first MC treatment in the year with no claims for MC agents in the preceding 12 months) and to survive ≥ 6 days after initiation. The first MC cycle started on the MC initiation date (day 1) and ended at the next administration at least 6 days, but no more than 35 days, after initiation. If no second cycle started before day 35, the first cycle was considered completed at the earliest of day 35 after initiation, the day before regimen change, death, disenrollment from Part A or B, or September 30, 2015.
Chemotherapy regimen was defined based on MC agents on Part A outpatient (OP) or Part B (PB) claims from day 1-day 6 of the first cycle and, on the same claims, an ICD-9-CM diagnosis code for NHL. Based on the National Comprehensive Cancer Network guidelines, regimens with FN risk >20% and 10%-20% were classified as high and intermediate FN risk categories, respectively. Patients receiving MC agents but not high or intermediate FN risk regimens were classified as "Other" FN risk category. PP-GCSF use was defined as an administration of pegfilgrastim or any short-acting CSF (filgrastim, tbo-filgrastim, filgrastim-sndz, or sargramostim) in OP/PB claims up to 5 days after first cycle chemotherapy completion. NP-related hospitalization was identified from Part A inpatient claims with ICD-9-CM diagnosis code 288.0X in the first five positions between day 7 and the last day of the cycle. We describe trends in proportions of patients receiving MC regimens by FN risk category, with PP-GCSF use, and with NP-related hospitalization in the first cycle. Trends in NP-related hospitalization rates were further evaluated using a logistic regression model with calendar year treated as a continuous variable and functional form estimated by a penalized spline after adjusting for age, race, baseline hospital length of stay, baseline NP-related hospitalization, number of comorbid conditions, and MC FN risk category.
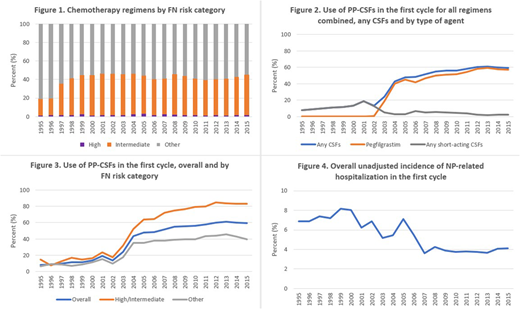
Results: Yearly cohorts included 538-717 eligible patients, 1995-2007, and 1877-2640, 2008-2015. Proportions of patients aged ≥80 years increased from 39% in 1995 to 44% in 2015. Proportions receiving high/intermediate FN risk regimens were <20% before 1997, 36% in 1997, and 40%-46% 1998-2015 (Figure 1). Most patients receiving high/intermediate risk regimens (88%-96%) received CHOP-21 (cyclophosphamide, doxorubicin, and vincristine every 21 days with or without rituximab).
Overall, PP-GCSF use increased from 8% in 1995 to 60% in 2015, mainly due to introduction of pegfilgrastim in 2002 (Figure 2). PP-GCSF use was more common in patients receiving high/intermediate FN risk regimens than in patients receiving other regimens (Figure 3). Overall, unadjusted incidence of NP-related hospitalization decreased from 7% in 1995 to 4% in 2015 (Figure 4). Change point in trend was detected at 2010; incidence of NP-related hospitalization decreased, on average, 6% each year before 2010 (p<0.0001) and was flat from 2010 (p=0.6) after adjustment for changed patient characteristics.
Conclusions: Among older patients diagnosed with NHL receiving MC, 1995-2015, PP-GCSF use increased substantially after 2002. Over the same 20-year period, incidence of NP-related hospitalization in the first cycle decreased, on average, 6% each year before 2010 and was flat from 2010. Further studies are needed to understand overall decreasing trends in NP-related hospitalization and effects of changes in chemotherapy and FN management.
Liu:FibroGen Inc.: Consultancy. Gawade:Amgen: Employment, Equity Ownership. Kim:Amgen: Employment, Equity Ownership. Bensink:Amgen: Employment, Equity Ownership. Chandler:Amgen: Employment, Equity Ownership.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal